Home health agencies and post-acute clinicians have started to prepare and educate themselves for what will be the most significant regulatory and reimbursement reform since the creation of the Prospective Payments System 20 years ago. The Patient-Driven Groupings Model (PDGM) is scheduled to become effective on January 1, 2020 and is being implemented as a more refined version of the much-debated Home-Health Groupings Model put forth by the Centers for Medicare & Medicaid Services (CMS) in early 2018. Although disruption is expected as the rollout occurs, the intent of PDGM is to reduce volume-based reimbursement that doesn’t necessarily align with a patient’s condition and for home health agencies to develop closer, more collaborative relationships with hospitals and skilled nursing facilities.
Overall, PDGM presents a challenge and an opportunity for home health agencies to transform their operating model to be more aligned with evolving value-based care initiatives already underway in the broader US healthcare industry.
What is Changing with Payment Reform?
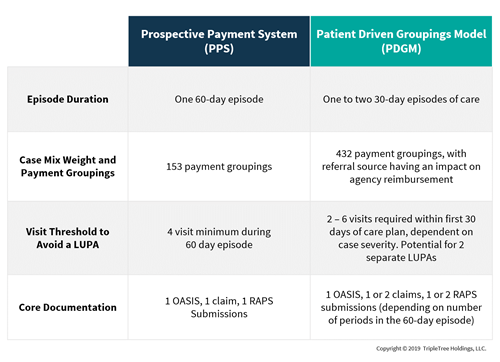
Prospective Payments System vs. PDGM
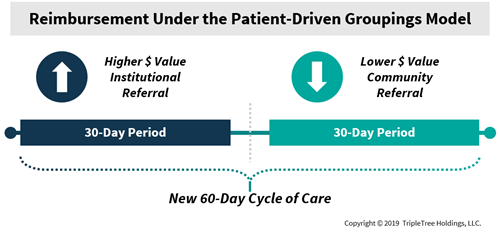
The headline change under PDGM will be the break-up of the standard 60-day episode of care into one or two 30-day periods, with the patient referral source having an outsized impact on the reimbursement amount a home health agency receives. More often, a patient is referred to a home-based care setting from an institution such as a hospital or health system following an acute care event, or from a skilled nursing facility, while others are referred from community providers, such as a primary care physician. The first 30-day episode referral source can be classified as either institutional or community, while all subsequent 30-day episodes in a consecutive stay will be classified as community-referred. As such, smaller agencies in rural markets will stand to feel more financial pressure as many of their patients are initially referred from community-designated sources, which garner less reimbursement under PDGM.
PDGM will further complicate the clinical documentation process by increasing the number of payment groupings and unique case-mix potential from 153 to 432, eliminating therapy volume thresholds as the primary determinant of reimbursement, while also changing the minimum number of visits that trigger a low-utilization payment adjustment (LUPA).
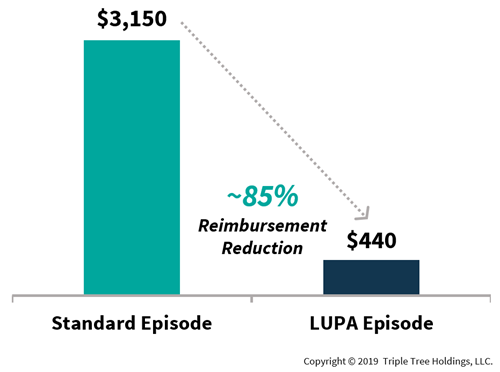 *Standard episode represents average reimbursement garnered by an appropriate utilization level over a 60-day period of care, and LUPA episode reimbursement represents the average FFS rate per visit multiplied by the number of visits that trigger a LUPA
*Standard episode represents average reimbursement garnered by an appropriate utilization level over a 60-day period of care, and LUPA episode reimbursement represents the average FFS rate per visit multiplied by the number of visits that trigger a LUPA
More controversially, although the proposed program is “budget neutral”, home health agencies are slated to experience a -6.42% behavioral adjustment as CMS assumes agencies will change diagnosis codes and add visits to reduce LUPAs.
 Operational Considerations and Opportunities for Home Health Agencies
Operational Considerations and Opportunities for Home Health Agencies
The home health agency operating model will need to adapt to the PDGM paradigm in numerous ways. With the amount of care time in the episode shrinking from 60 days to 30 days, the first 24 – 48 hours of the episode will be crucial for the home health agency to document the patients’ care plan and to assess the level of resources that the patient will need throughout the episode. With the removal of therapy visits as a determinant of reimbursement, agencies will need to stay on top of care plans and in-home assessments to optimize reimbursement.
Clinical documentation surrounding the Outcome and Assessment Information Set (OASIS) will need to be enhanced to adhere to new payment grouping standards and to substantiate the care plan. Furthermore, with the LUPA threshold changing from a “bright-line” 4 visits minimum to a range of 2 - 6 visits within each 30-day period, the patient severity will need to be appropriately documented and updated throughout the full 60-day cycle.
Finally, the staffing model of agencies will need to be enhanced. With the number of claims and the Risk Adjustment Processing Systems (RAPS) submissions nearly doubling under PDGM, additional staff will be required to process claims and agencies will need to re-evaluate the amount of Medicare dollars that each biller can process and collect.
In this new era of value-based care and payment reform, there is a significant opportunity for RCM vendors to proactively identify transitional pain-points that home health agencies may experience. Vendors such as
McBee Associates have already been conducting PDGM impact assessments and devising new operational playbooks for agencies to help successfully navigate the upcoming transition. McBee is also using a vast repository of Medicare claims data in unique ways to assess an agency’s financial impact under new payment models and policy scenarios.
Our Take
Along with the challenges that payment reform will bring, opportunity will follow. Over the past 20 years, home health providers have proven they can effectively evolve their operating models to navigate evolving regulatory dynamics. PDGM will further drive value-based care initiatives across the care continuum, and enable more collaborative relationships between institutions and home health agencies. However, the initial disruption caused by PDGM also brings opportunities to larger providers such as
Amedisys,
Kindred at Home,
Elara Caring and
AccentCare, who have the operational scale to drive further consolidation in the industry. These larger organizations could find more M&A opportunities for smaller groups who may face disproportional headwinds under the new reimbursement model. Finally, RCM service providers stand to gain influence among industry stalwarts and implement best-practices in the years to come as the post-acute care market continues its upward growth trajectory.